Strengthening Health Systems for Resilience in Times of Change
by Skylar Yan, CCIH Intern
“I can do all things through him who strengthens me.” -Philippians 4:13
Ever since the era of COVID-19’s beginning, there have been numerous struggles throughout the international Christian community. Faith fell to an all time low, churches and communities were unable to meet and many remained isolated at the time. At the same time, the healthcare industry received a massive wave of people in need, while being extremely understaffed.
Although it’s uncomfortable to look back on these earlier days of the COVID-19 years, they also raised an important question: How can we as the Christian health community better prepare ourselves for these types of crises? In the June 16th session of the CCIH 2022 Conference, we tackled strengthening health systems for resilience in times of change.
Building Resilience with Training
No matter what the context, resilience is vital to overcoming challenges, and to react to and recover from natural disasters, conflict and other devastating events. In the fourth session of the CCIH 2022 Conference on July 16, we started the discussion on strengthening health systems with an interview of Dr. Nathaniel Smith, MPH, Centers for Disease Control and Prevention (CDC), by CCIH Executive Director Doug Fountain (below).

When asked how the CDC was strengthening health systems, he spoke on their recent training approaches. The CDC is currently addressing the two current problems of adaptability and surge capacity, both of which can be addressed through workforce advancement. By having more people trained in the basics of healthcare, specialized training takes less time and teams can respond to health crises faster and more efficiently.
Some examples of the CDC’s training programs include an epidemiology training program and a Laboratory capacity training program, which both seek to quickly develop qualified workers to make up for gaps in the workforce. Not only does the CDC look to expand their own workforce, but also seeks to assist public health authorities with emergency assistance in times of crisis.

Turning to Sierra Leone and examples of partnerships among local actors and health workers from the U.S., we heard from Dr. Gary Gilkeson, Dr. Aruna Stevens, Chief Medical Officer, Mercy Hospital in Bo, Sierra Leone, (above) and Yasmine Vaughan, MPH, Technical Advisor for Global Health and Missions, Helping Children Worldwide. In an under-resourced country like Sierra Leone, health facilities are often understaffed and health workers lack modern training and techniques. By partnering with external healthcare professionals, new healthcare workers can be trained quickly and efficiently. Teams of international surgeons bring new and modernized techniques to further the repertoire of already experienced surgeons.
Lisa Ailaniello, RN, MSN, Director, Medical Benevolence Foundation Center of Global Nursing Development; and Philemon Mulenga, BS Nursing, Nurse Midwife and Training Officer, Christian Health Association of Malawi; (below) further expanded on the theme of training with their presentation on e-learning.

By using Moodle, they were able to create an e-learning program that could be personalized for nine higher education schools. With 24/7 technical support, efficient curriculum implementation, and a viable supporting infrastructure, this e-learning platform is still being used even after the pandemic and provides a stable alternative to in-person learning.
The conference session on health system strengthening also brought to light some flaws in current healthcare training, while also proposing solutions to these problems. In his presentation, Dr. Timothy Nunn, Medical Director, CURE Ethiopia pointed out that there was a lack of and a need for holistic training in residency. During his research, he found that ethics was a heavily overlooked part of training. He pointed out that violating good ethics is hurting patients, while also showing the low costs it would take to implement ethics training. Because it’s not technical, ethical training would take less time to implement, would be low cost, and would be useful in surgery and in one-on-one patient care.
Father John Varghese, (above) working at St. John’s Hospital (based in Bangalore in India) also pointed out the lack of technical literacy and trainers. However, thanks to the commitments the hospital made in the CCIH’s 30×30 Health Systems Initiative there have been over a hundred new workers trained and a universal healthcare ID for each patient throughout India.
Resilience through Technology
Technology was also a key factor in the resilience discussion. Dr. Stephen Letchford of Banda Health (SIM) and Diana Ayabei of the SpaceCare Medical Clinic in Kawangware, in Nairobi, Kenya (below) showcased the power of infrastructural advancements through the project Banda GO.

Banda GO is a healthcare system created by Banda Health that empowers clinics to efficiently find patient records. Banda GO has been set up in more than 70 frontline clinics, and also helps prevent theft, access medical notes quicker, and completes outpatient reports in less than five minutes, a task previously tedious and time consuming. Ms. Ayabei shared her experiences with Banda GO, and as she runs the only health clinic in Mtego Estate Nairobi, it has revolutionized not just the workers, but also their patients’ outlook on healthcare.
While Banda GO focuses on the patient and records side of technology, Richard Neci Cizungu, Executive Director, Ecumenical Pharmaceutical Network, Joseph Rugut, Biomedical and Renewable Energy Engineer, Christian Health Association of Kenya, and Saona Phiri-Ndhlovu, Manager of Storage and Distribution, Churches Health Association of Zambia (below) focused on the supply chain.

When asked how to keep the supply chain resilient, they used the oxygen problem as an example. During the COVID-19 pandemic, oxygen became a precious commodity. The oxygen itself wasn’t an issue, but the equipment and the cylinders needed for oxygen storage were insufficient and costly to produce. Together, through clever engineering and revisited concepts, they were able to create a new, more efficient oxygen cylinder that greatly bolstered the oxygen supply and made their rounds towards hospitals.
Resilience through Faith and Community
Although training and technology took the stage that day at the conference, resilience from the faith community in general was also a hot topic. Dr. Esther Kuhn, Senegal Country Director, World Renew (below) showcased the adolescent’s health and rights program and its results for the community. The program, designed for adolescent women uses a community-based approach to change behavior and increase effective communication.
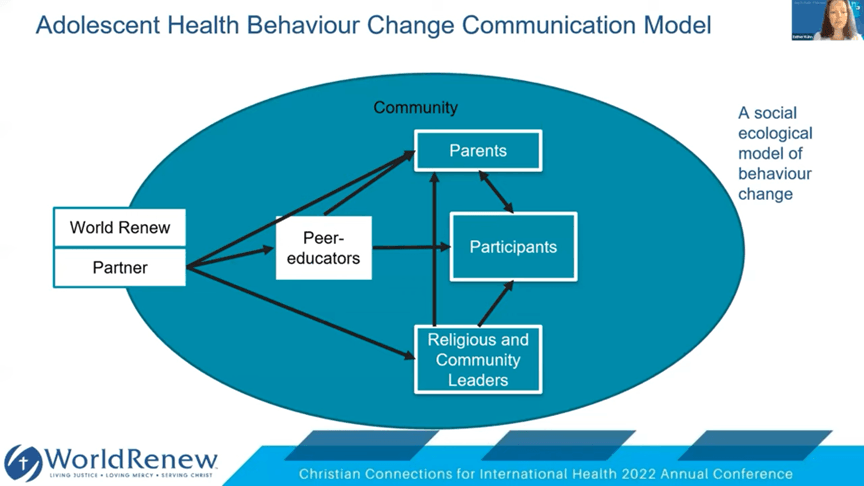
Through peer-to-peer communication, adolescents are introduced to group work, skits, and discussions of topics relating to faith and maturity. This program not only led to healthy relationships, fewer teen pregnancies, and prevention of domestic abuse, but also garnered them esteem in their respective communities. Parents became more willing to listen to their children and increase their decision making, allowing them to become established members of their community. While starting off in Senegal, this program has also spread to Nigeria, Niger and Bangladesh.
Through this variety of programs in different parts of the world, we got a view into what faith-based organizations are doing to strengthen the health systems where they work, enabling to reach more people effectively with care. If you missed the session, please visit the CCIH YouTube Channel for the 2022 Conference Playlist.
About the Author: Skylar Yan is a CCIH Intern and a third year Economics major at Pepperdine University. As an aspiring young researcher, he hopes to one day combine his passions for economics and healthcare to create an impact in the world.